Introduction
Millions of people worldwide suffer from poor blood circulation in their limbs, often without realizing the underlying cause. One of the most common vascular conditions responsible for this is peripheral artery disease (PAD), a health issue that affects the arteries outside the heart and brain, especially those supplying the legs and feet. If left untreated, peripheral artery disease can lead to pain, mobility issues, and in severe cases, serious complications like tissue damage or even amputation. Understanding the symptoms, risk factors, and available treatments for PAD is crucial for maintaining good vascular health and preventing long-term problems.
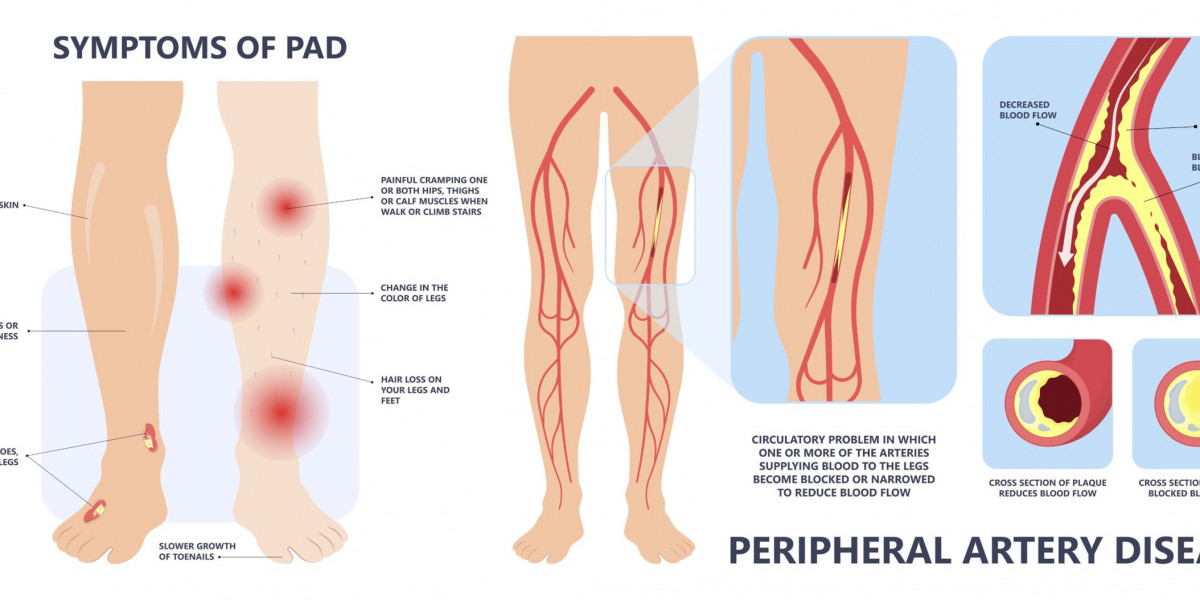
What Is Peripheral Artery Disease?
PAD refers to the narrowing of the peripheral arteries, most commonly in the legs. The main culprit is a buildup of fatty plaques (atherosclerosis) on the inner walls of these vessels. Over time, plaque narrows the arteries, reducing blood flow and oxygen delivery to tissues. This process affects anywhere from the hips to the toes, leading to a range of symptoms and complications.
Risk Factors for PAD
PAD shares many risk factors with heart disease. Some key factors include:
Age: Risk increases in people over age 50.
Smoking: One of the most significant contributors—a major accelerant of arterial damage.
Diabetes: High blood sugar levels damage blood vessels.
Hypertension: Elevated blood pressure contributes to endothelial damage.
High cholesterol: More plaque build-up in arterial walls.
Obesity & Sedentary lifestyle: Increase cardiovascular strain and reduce blood flow.
Family history: Genetic predisposition may heighten risk.
Chronic kidney disease: Often coexists with vascular dysfunction.
Symptoms to Watch For
Symptoms may range from mild to severe. Common early signs include:
Claudication: Painful cramping in the legs or hips while walking, as muscles don’t receive enough blood.
Numbness or weakness: Weakness in leg muscles or loss of sensation.
Coldness in lower leg or foot: Especially when compared to your other side.
Sores or wounds: Wounds on toes, feet, or legs that heal slowly or not at all.
Change in foot color: Pale, bluish, or glossy skin indicates poor circulation.
Shiny skin and hair loss: Reduced hair growth on legs and toenails and thinning, shiny skin.
Weak pulse: In legs or feet.
As PAD progresses, resting pain and gangrene may occur. Severe PAD can lead to amputation or critical limb ischemia.
How Is PAD Diagnosed?
Screening and early diagnosis are key. Healthcare providers use:
Medical History & Physical Exam
Discussion about symptoms, risk factors, lifestyle.
Palpation of pulses in legs and feet.
Ankle-Brachial Index (ABI)
Blood pressure measured in the ankle and arm.
An ABI ratio below 0.90 suggests PAD.
Doppler Ultrasound
Visualizes blood flow and identifies blockages.
Angiography
Uses contrast dye with X-ray, CT, or MRI to highlight blood vessels.
Offers detailed visualization for treatment planning.
Blood Tests
Assess cholesterol, glucose, kidney function, and markers of inflammation.
Treatment & Management Options
PAD management is tailored based on severity and individual health. Main strategies include:
Lifestyle Modifications
Quit smoking: Most effective single action—dramatically improves circulation and slows disease progression.
Exercise regularly: A supervised walking program helps improve pain-free walking distance.
Healthy diet: Focus on fruits, vegetables, whole grains, lean proteins, and low saturated fats.
Weight management: Helps ease strain on your heart and arteries.
Medications
Antiplatelet agents: Aspirin or clopidogrel reduce clot risk.
Cholesterol-lowering drugs: Statins reduce plaque buildup.
Blood pressure control: ACE inhibitors, beta blockers, or diuretics.
Blood sugar control: Metformin, insulin, or other diabetic medications.
Symptom relief: Cilostazol or pentoxifylline may improve walking distance.
Minimally Invasive Procedures (Endovascular)
Angioplasty: A balloon is inserted and inflated to open blocked arteries.
Stenting: Metal mesh tubes keep arteries open.
Atherectomy: Specialized devices remove plaque buildup.
Surgical Interventions
Bypass surgery: Redirects blood around blocked artery using a graft.
Living Well with PAD
Management extends beyond treatment. Long-term care strategies include:
Regular check-ups: Routine ABI tests and follow-up imaging.
Consistent medication use: Adherence helps prevent worsening or complications.
Symptom monitoring: Watch for changes like rest pain, non-healing wounds, or leg discoloration.
Foot care: Particularly vital for people with diabetes or neuropathy—inspect daily for sores or infections.
Smoking cessation support: Counseling or nicotine replacement for successful quitting.
Exercise maintenance: Consistency is key—structured walking improves vascular health.
Manage comorbidities: Keep blood sugar, cholesterol, and blood pressure under control.
Prevention: Stop it Before It Starts
Preventing PAD focuses on heart-healthy habits:
Don’t smoke.
Eat a balanced, nutrient–rich diet.
Stay physically active—150 minutes of moderate aerobic activity weekly.
Maintain optimal weight.
Regular medical screenings, especially if you have diabetes, high blood pressure, or high cholesterol.
When to See a Doctor
See your provider if you experience:
Leg or foot pain, cramps, numbness, or weakness during activity.
Persistent temperature differences or color changes in your legs.
Sores on the feet or legs that don’t heal in two weeks.
Increased pain at rest or during the night.
Frequently Asked Questions (FAQs)
Can PAD affect parts of the body other than the legs?
Yes. While most common in legs, PAD can also impact the arms, pelvis, or kidneys.
Is PAD the same as peripheral neuropathy?
No. PAD involves blood flow issues, whereas peripheral neuropathy involves nerve damage. Though they can coexist—especially in diabetes—the causes and treatments differ.
Can PAD lead to heart problems?
Absolutely. PAD is often a marker of widespread arterial disease, increasing the risk of heart attacks and strokes.
Can PAD be fully reversed?
The goal is to manage and reduce progression. While lifestyle changes, medications, and procedures can significantly improve symptoms and functionality, the underlying arterial changes may not be fully reversed.
Conclusion
Peripheral artery disease is a widespread condition with serious consequences—but it doesn’t have to define your quality of life. Awareness, early detection, and proactive management enable you to lead an active, fulfilling lifestyle. Whether it’s adopting a clean, healthy diet, quitting smoking, or committing to a supervised exercise plan, the steps you take today can safeguard your vascular and overall health tomorrow.